Picky Eating vs ARFID: What Every Parent Needs to Know
- rachel76931
- May 31
- 6 min read
If I had a dollar for every time someone told me, “They’ll eat when they’re hungry,” I’d have enough to fund a nationwide campaign on why that advice just doesn’t work for neurodivergent kids or children with ARFID.
Because not all picky eating is created equal.
Some kids avoid broccoli for a while, then move on.
Others survive on beige foods, gag at the smell of cooking, or scream if foods touch on the plate.
If that sounds familiar, this blog is for you.
Let’s explore what ARFID actually is, how it’s different from typical fussy eating, and - most importantly - how to support your child without the stress.
What is ARFID?
ARFID (Avoidant/Restrictive Food Intake Disorder) is a feeding disorder that’s often mistaken for “picky eating.” But it’s more than just preference - it’s a nervous system response.
These kids aren’t just choosy. They’re scared. Their brain sees food as a threat, and their body goes into survival mode.
The differences between ARFID and developmental picky eating
While typical picky eaters tend to have at least 20 foods, kids with ARFID usually have less (sometimes as few as 1 or 2)
Kids with ARFID often have strong anxiety and sensory food aversions
Typical picky eaters will usually still eat regularly without prompting, while ARFID kids often don't seem interested in eating.
And unlike picky eating, ARFID doesn’t go away on its own.

The diagnostic criteria for ARFID includes:
Significant weight loss or nutritional deficiency
Dependence on enteral (ie tube) feeding or oral nutrition supplements
Marked interference with daily functioning
Why “just keep offering” doesn’t work
Many people (including professionals in your child's life such as doctors or teachers) do not understand ARFID.
Let me gently call out some well-meaning (but totally unhelpful) advice:
“Just make them try one bite.”
“They’ll eat when they’re hungry.”
“You shouldn’t cater to them.”
These don’t work because ARFID is not a behavioural issue - or even a conscious cognitive 'choice'. They see the broccoli and literally feel like they are being chased by a tiger and so their nervous system goes into fight/flight ('tiger brain') or freeze/fawn ('turtle brain').
When this happens, eating feels impossible. So continuing to prompt or pressure the child to eat - especially without giving supports - will only make it worse. The goal isn’t to push the food or 'just get them to take a bite': it’s to calm the nervous and sensory systems to that eating feels safe again and curiosity can return ('Owl Brain').
What causes ARFID?
In most cases, ARFID is driven by a unique mix of:
Anxiety: Fear of choking, vomiting, or being sick. Maybe even the fear of the unknown.
Sensory Processing Differences: The textures, smells and temperature of the food feels overwhelming
Differences in Interoception: Not recognizing or interpreting hunger/fullness cues
Trauma or past negative food experiences
Neurodivergent kids are especially at risk because of their nervous and sensory systems are more sensitive to inputs (and eating is such as highly sensory experience).
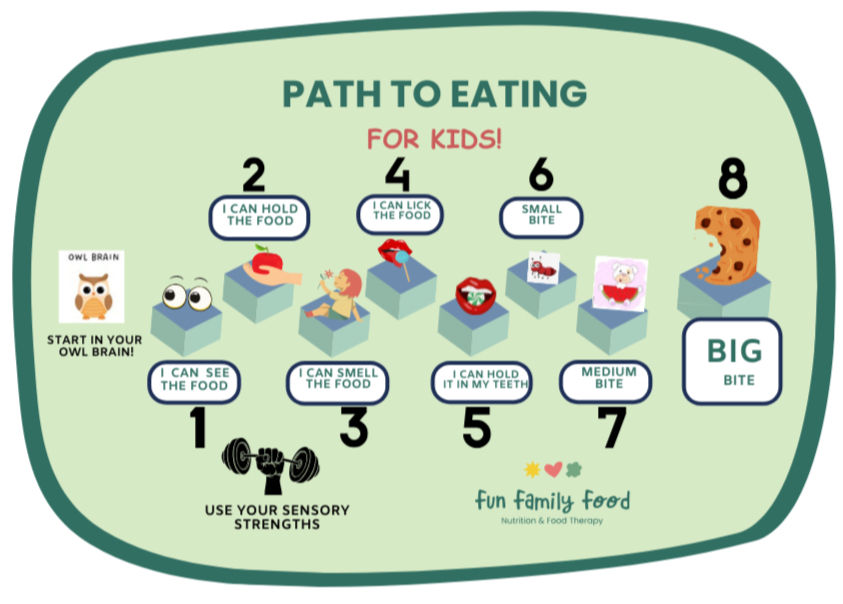
How I Help Kids with ARFID: The Path to Eating Framework
I have developed the Path to Eating Framework from hundreds of hours of feeding therapy supporting kids with ARFID (some of whom had only 1 or 2 foods). Time and time again I would see that we made zero meaningful progress until we calm the nervous system and get the child relaxed and engaged.
You can't achieve this with rigid protocols or even any set timeline. In fact, pushing ahead without the child being in 'Owl Brain' (calm-alert nervous system) can have disastrous consequences: I have supported many families who have 'tried feeding therapy' and didn't have results because it was simply a one size fits all protocol and didn't take the time to make sure the child was actually ready and engaged. Often, that history set the child back and made things harder.
Instead of trying to push food in, we invite curiosity out using my step-by-step Path to Eating.
Step 1: Prepare your child
Before we put a child anywhere near a new food, we work to regulate their brain and body - get their nervous system out of fight/flight and into calm-alert.
This will help them come to the meal feeling calm, confident and curious.
Regulate the body: A heightened child in 'tiger brain' might need to run, do some heavy lifting or push-pull work - anything to get the tension out of their big muscles. A child in 'turtle brain' might need some gentle activities to bring them out of their shell.
Pro tip: Spend at least 10 minutes before a mealtime using play to regulate their brain and body.
Other specific anxiety and mealtime strategies: depending on the age of the child and their presentation, tools such as:
Sensory preparation and sensory accommodations at mealtimes (check out the Neurodiverse Kids Guide to Mealtimes for ideas)
Supporting Responsive Feeding: Removing pressure, giving the child autonomy, teaching skills and being attuned to your own unique child
Developing flexible routines and working towards the Division of Responsibility in feeding (ARFID kids often need extra scaffolding and supports before this can be implemented in full).
Optimising the mealtime set up (this can look different for every family), using language that lowers anxiety, finding a mealtime system that meets the needs of that child.
Using co-regulation: kids who are anxious often can't 'calm down' on their own, they need to 'borrow' the calm nervous system of a trusted adult.
....and many more.
Step 2: Assess and Understand
In practice I find most cases of ARFID are due to their own unique combination of all three potential causes. There is no 'one size fits all' plan or protocol that helps every child.
If we can get to the bottom of what's really going on for the child, and combine that with a deep understanding of their strengths, interests, skills, motivations, family situation, current and past foods eaten and more, we can find their quickest path to eating.
Step 3: Try New Foods
Learning to eat new foods can be like learning to read or learning to swim. There's lots of little micro-skills that need to come together first.
Did you know there are at least 32 micro-steps in the process of eating, and that it takes most typically developing kids at least 2 years to master them all: from learning to coordinate the suck/swallow of milk to eating a variety of foods from the family's diet.
The Path to Eating draws on the concepts in widely used therapy frameworks (such as Sequential Oral-Sensory or SOS; food chaining and more) - always underpinned by the principles of responsive feeding.
I use the formula of:
PLAY + CHILD's INTERESTS to help them move through the steps.
STEP 4: Help and Support
You are with your child 24/7: Teaching you the tools and strategies (and helping implement them) is the most effective way.
Want to Try This at Home? Here Are 5 Simple Wins
You can start helping your child with food today with these strategies:
Validate their feelings:
“This feels tricky for you right now” instead of “Just eat it!”
Take eating off the table:
“You don’t have to eat it - let's just meet the food first.”
Play with food:
Bring out some kitchen utensils and let them chop, squeeze and explore. Even if they don't eat the first few times (they probably won't!), each play based exposure is rewiring their brain and calming that nervous system response.
Use sensory language: This takes the judgement out of it and keeps things neutral: "Is it hard or soft?” “This food feels as soft as a cloud!”
Try one new food as a family: Every week while shopping, buy one new or different food. Put it on a plate in the middle of the table, print out my ARFID Placemat and let curiosity do its thing.
Your next step: watch my free 10 minute Masterclass
If you are concerned about your child's eating, I made a 10-minute video showing you how my feeding program Nourish Empower Thrive works to support kids with ARFID.
It walks you through:
✔ Why your child isn’t eating
✔ What actually works
✔ How to help without harming
Final Thought
There's often lots of feelings that come up when your child has been diagnosed with ARFID:
Relief from guilt and self blame: there's nothing you could have done differently
Reduced frustration: knowing that your child literally feels like food is life or death and their responses are just their body trying to protect them helps to externalise the eating disorder behaviours you see on the surface.
Grief from how you thought feeding would look
Validation: this is why it has felt so hard to feed your child
....and hope: ARFID is tough, but recovery is possible.
If you suspect your child has ARFID or you are concerned about their eating, your GP is your first port of call.
You can also check out my free guide 'Overcoming ARFID and Extreme Picky Eating' and follow along on Instagram for tips and support.
Ready to get specialised feeding support for your child? Don't hesitate to reach out: rachel@funfamilyfood.com.au
Disclaimer: The information in this blog is general in nature and is not intended to constitute or substitute for professional or medical advice. You should seek appropriate professional advice suitable for your personal circumstances.

Comments